
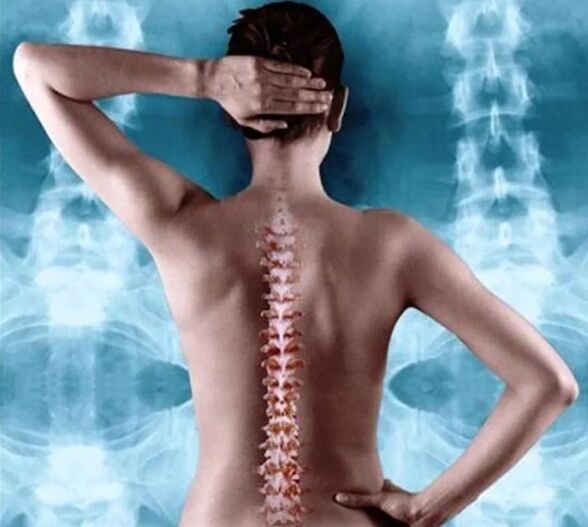
The human spine is one of the most important components of the musculoskeletal system, and a violation of its normal functioning always causes negative consequences for the whole organism. Thoracic osteochondrosis refers to degenerative-inflammatory diseases of the spinal discs in the thoracic region. The disease most often affects people over the age of 55, but it can also occur in any adult. In men, the disease is registered half as much as in women.
In general, although the department is the largest, consisting of 12 vertebrae in the center of the spine, it is less prone to pathologies. This is due to the reduced mobility and good protection of the muscle corset. This feature of the structure is a positive factor, but in the diagnosis of osteochondrosis of the thoracic region it is difficult to identify and can be confused for a long time with other diseases, especially when there is a temperature.
There are criteria for the 10th revision of the International Classification of Diseases (ICD-10), according to which osteochondrosis belongs to the class of dorsopathy (M40-54). There is a separate class of ICD-10 for osteochondrosis of the spine - M42 according to ICD-10 and is equated with deforming dorsopathies. Diagnosis is made according to the M42 code. 0 ICD-10 for young people and M42. 1 ICD-10 for adult osteochondrosis. The code M42. 9 ICD-10 can occur with unspecified pathology.
The reasons
Thoracic osteochondrosis is less common than injuries in other parts of the spine. Many people have not sought medical attention in a long time, thinking they have other medical conditions. According to statistics, this leads to the detection of the disease most often in an advanced form.
The disease occurs due to impaired nutrition and blood supply to the intervertebral discs. The formation of osteochondrosis can lead to disruption of the normal structure of the vertebrae. The elasticity and depreciation properties of the spine are lost, and all this leads to the destruction of discs, ligaments and other structural components. As a result of such ailments, the nerve roots are pinched and unpleasant symptoms occur.
It is almost impossible to find out the exact causes of the pathology. There is a risk group between people and the predisposing factors that lead to the disease. As for the people themselves, this age is more than 55 years old, female sex and the presence of spinal pathologies increase the risk of getting sick. Deviations such as scoliosis, kyphosis, over time, violate the posture and normal arrangement of the spine. As a result, the metabolic processes in the spine are disturbed and chondrosis is formed.

There are factors directly dependent on the person that lead to the disease. We highlight the main ones:
- excess body weight;
- abuse of bad habits: alcohol, smoking, fatty foods;
- sedentary lifestyle.
People who spend a lot of time in a sitting position are prone to the disease. This applies to employees, seamstresses, operators, drivers. A person who has suffered a back or spine injury should also be careful in the future. There is a group of people with hereditary or acquired diseases who are prone to diseases of the musculoskeletal system. The main conditions are diabetes mellitus, muscle weakness, disruption of the normal functioning of the glands.
Types and clinical picture
Signs of osteochondrosis of the thoracic spine depend on the degree of pathology and the neglect of the process. In total, four degrees of the disease are distinguished.
At the first degree, there is a violation of the elasticity of the intervertebral discs and a decrease in their height. Pain symptoms are not as acute and quickly pass to rest. Basically, the pain is felt in the middle of the back and chest. Often the disease passes into a passive state, and clinical manifestations appear only during exacerbation, quickly stopping and treatable. Signs of intoxication are rarely present, sometimes the temperature may rise and weakness may occur. The temperature quickly normalizes as the acute period passes.
The second degree is more dangerous and can cause severe neurological symptoms. With this degree, the height of the discs of the spine constantly decreases, the elasticity is broken. The fibrous ring of the intervertebral disc can be damaged and a crack forms. This stage is fraught with the threat of the appearance of an intervertebral hernia.
The pain in the chest and back becomes stronger and eventually spreads to the adjacent area. During deep breathing or sudden movement, a sharp attack of pain occurs. When nerve endings are damaged, symptoms spread along the ribs. During the period of exacerbation, there is an increase in temperature, general weakness. With this degree of disease, a feeling of numbness and creeping "goosebumps" joins the site of the injury. If the nerve fibers are damaged, the normal innervation of the upper or lower extremities is disturbed.
Osteochondrosis of the thoracic region of the third degree is characterized by the onset of the formation of an intervertebral hernia. There is severe pain that occurs under certain circumstances. Often the pain can intensify at night, when standing in the cold for a long time, in one position. Pain in the chest, back, along the ribs. When exposed to the spinal cord, the following symptoms may occur:
- violation of the innervation of the legs and arms;
- increased pain at night;
- pain in the esophagus, right hypochondrium, stomach;
- increase in body temperature;
- problems with the normal functioning of the gastrointestinal tract.

In the last, fourth degree, the bone tissue of the spine is destroyed. There is a violation of the mobility of the vertebrae, the depreciation properties are reduced. Thoracic osteochondrosis in this degree is dangerous due to damage to the spinal cord and impaired human performance. With an exacerbation, the body temperature rises, there is severe pain in the chest, in the middle of the back.
In the general clinical picture, two main symptoms are distinguished: dorsago and dorsalgia. Dorsago is characterized by severe pain in the chest. A person has the sensation of shooting in the chest after a long stay in one position. During an attack, breathing becomes difficult and the pain intensifies with the movements of the torso to the sides. This condition raises the temperature.
With back pain, there is slight pain in the area of the damaged vertebrae. Pain symptoms increase and last up to three weeks. The pain becomes stronger after a deep breath or an exhalation and with movements. Symptoms worsen at night and are relieved by walking. The 10th revision of the International Classification of Diseases (ICD-10) assigns a separate code M54. 6 to back pain with chest pain.
Diagnosis and treatment
Thoracic osteochondrosis with the right approach is not difficult to identify. The main thing is to conduct a differential diagnosis with cardiovascular pathologies and to exclude other diseases. The presence of specific pain, fever and neurological disorders increase the doctor's doubts.
The main diagnostic method is radiography. It is necessary to take a picture not only of the damaged department, but also to capture the adjacent ones in order to exclude complications. If it is impossible to fully examine the spine and if tissue and vascular damage is suspected, computed tomography and magnetic resonance imaging are prescribed.
Thoracic osteochondrosis in most cases is treated with conservative methods.
The main thing in the treatment is the complexity and individual approach.
Depending on the degree of pathology, a home treatment regimen or a hospital is possible. In any case, it is necessary to apply certain principles - this is a gentle load regime, which limits weight lifting and sports practice, preventing overwork and strict adherence to the doctor's recommendations.
Thoracic osteochondrosis in the acute period of the disease, when there is pain, temperature, requires bed rest. NSAIDs, analgesics are prescribed when pain and temperature syndrome are present. Perhaps a combination of ointments, physiotherapy and massage. This combination will allow you to quickly overcome the disease and get back on your feet.
The basis of the treatment of osteochondrosis is a local effect. Manual therapy will allow to put the vertebrae in place, massage, physiotherapy (electrophoresis, ultrasound, magnetotherapy) and reflexotherapy can restore nutrition. It is important that both men and women engage in therapeutic exercises and adhere to the treatment regimen.
With complications, traction or even surgery may be prescribed. If not, symptomatic therapy is used.
























